Probiotics Made You Worse? Meet Parabiotics — A Gentler Option for IBS and Sensitive Guts
If you’ve spent any time researching gut health, you’ve probably come across the terms probiotics and prebiotics. In recent years, a third term has started to emerge in both the research and clinical space: parabiotics.
While these words are often used interchangeably, they are not the same thing. Understanding the difference between probiotics, prebiotics and parabiotics can make a significant difference to how you support your gut — particularly if you experience IBS, bloating, pain, or react badly to many supplements.
This article will break down what each one is, how they work in the body, and why parabiotics are gaining attention as a gentler, more targeted option for people with sensitive digestive systems.
What are probiotics?
Probiotics are live bacteria or yeasts that provide a health benefit when consumed in adequate amounts. These are often referred to as the “good bacteria”, but their role goes far beyond digestion alone.
A healthy and diverse probiotic population helps to:
Support digestion and nutrient absorption
Produce certain vitamins, such as vitamin B12 and vitamin K
Regulate immune function (around 70% of the immune system resides in the gut)
Compete with harmful microbes for space and nutrients, which prevents them from overgrowing
Produce antimicrobial compounds that help keep opportunistic organisms in check
When probiotics are present in balanced numbers, they contribute to a stable and resilient gut ecosystem. This balance is essential for reducing inflammation, supporting gut barrier integrity, and maintaining overall health.
It’s important to understand that most probiotic supplements do not permanently colonise the gut, if you stop taking probiotics they are gone after about 2 weeks. Instead, they act more like visitors — influencing the existing microbiome as they pass through, then exiting the body. This is why strain selection, dosing, delivery method and research evidence are all critical when choosing a probiotic. And this why I also have new patients tell me probiotics have not helped, but they find my practitioner-prescribed probiotics at the right dose gives them symptom relief.
What are prebiotics?
Prebiotics are types of fibre and resistant starches found in carbohydrate-containing foods that we cannot digest ourselves. Because they pass through the small intestine intact, they arrive in the large bowel where they become food for our beneficial bacteria. The more variety of fibres and starches you eat, the more diversity in your microbiome, which leads to positive health outcomes.
Once your bacteria eat and ferment prebiotic fibres, they produce compounds called short-chain fatty acids (SCFAs), including butyrate, acetate and propionate. These compounds are essential for gut health.
SCFAs help to:
Nourish the cells lining the colon
Maintain the integrity of the gut lining
Reduce intestinal permeability (often referred to as “leaky gut”)
Modulate inflammation and immune activity
In simple terms: prebiotics feed probiotics, and probiotics then create beneficial compounds that support gut and whole-body health. ( We can actually measure your microbiomes potential to produce SCFA’s via stool testing).
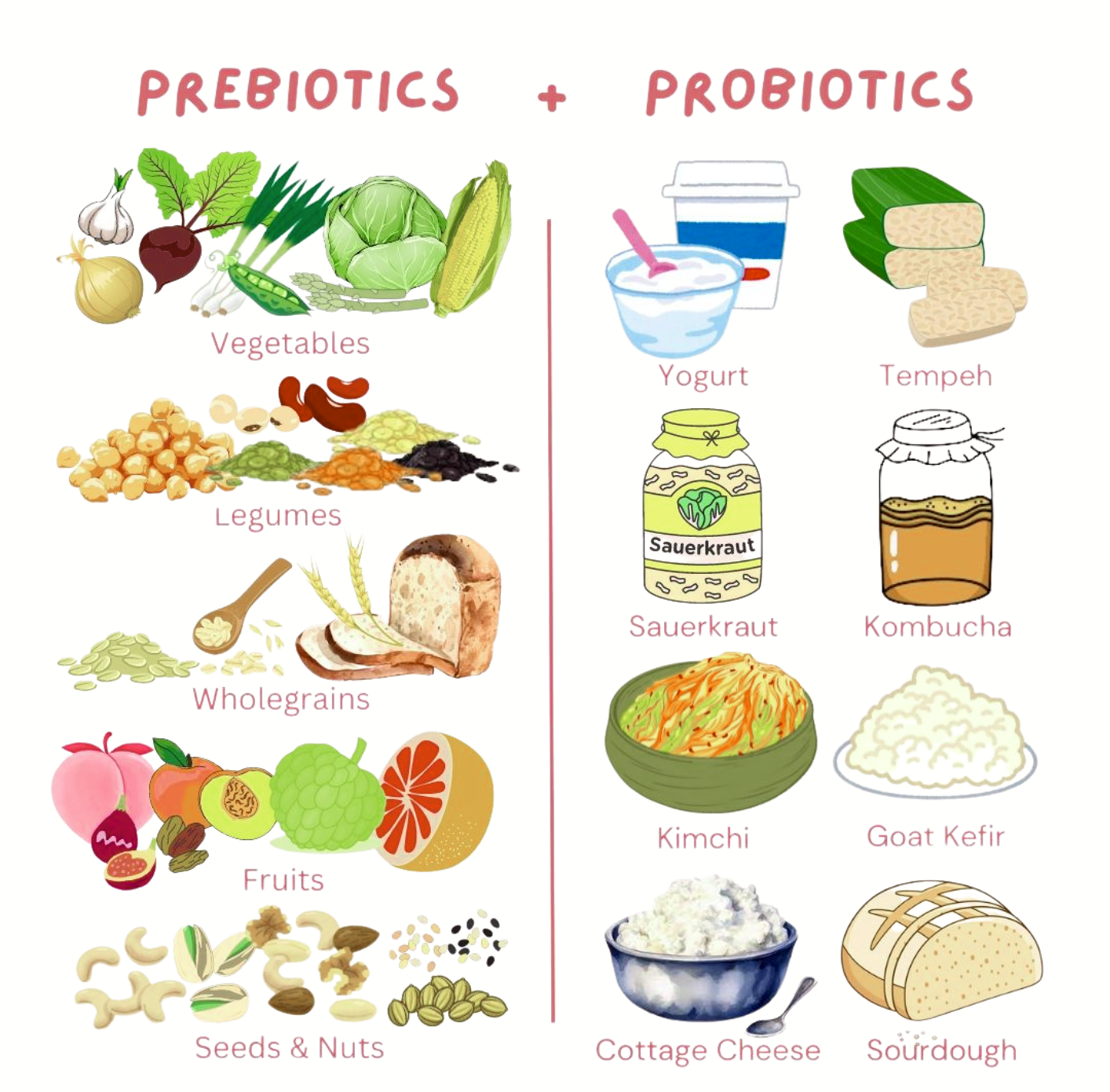
Food sources of probiotics and prebiotics
Probiotic-rich foods
We begin developing our gut microbiome from the moment we are born. Over time, diet, environment, medications (especially antibiotics), stress and illness all shape the balance of our gut bacteria.
Probiotic foods include:
Yoghurt with live cultures
Kefir
Sauerkraut
Kimchi
Kombucha
While these foods can be supportive, they are not suitable for everyone. Some people with histamine intolerance, SIBO or significant gut inflammation may find that fermented foods worsen symptoms.
Prebiotic-rich foods
Prebiotics are found in a wide variety of plant foods, particularly fruits and vegetables. Variety matters just as much as quantity, as different fibres feed different strains of bacteria.
Some of the richest prebiotic foods include:
Chickpeas and legumes
Asparagus
Green (unripe) bananas
Jerusalem artichokes
Apples
Onions, leeks and garlic
Dandelion greens
For people with bacterial overgrowth or dysbiosis, these foods can sometimes trigger bloating, pain, excess wind or foul-smelling gas. In these cases, the issue is not the food itself, but the underlying imbalance. This is where personalised guidance becomes essential. We need to address the underlying balance and then build up a healthy microbiome while slowly re-introducing all these foods again.
So what are parabiotics?
Parabiotics are a newer and rapidly emerging area of gut health research. They refer to non-living (inactivated) probiotic organisms or their beneficial components that still exert positive effects on the body.
In other words, parabiotics are probiotics that have been heat-treated or otherwise inactivated, meaning they are no longer alive — but they are still biologically active.
This might sound counterintuitive at first. After all, haven’t we been told for years that probiotics must be alive to work?
Research is now showing that many of the benefits of probiotics come not from their ability to colonise the gut, but from:
Their cell wall components
Their metabolites, which provide chemical messages
Their interaction with immune and gut lining cells
Parabiotics allow us to harness these benefits without introducing live organisms into an already sensitive or unstable gut environment.
How parabiotics can help gut symptoms
Parabiotics are particularly useful for people who:
React badly to traditional probiotic supplements or foods
Experience worsening of bloating or pain with live bacteria
Have SIBO, fungal overgrowth or recurrent infections
Have highly sensitive or inflamed gut linings
Potential benefits of parabiotics include:
Supporting gut barrier integrity
Modulating immune responses in the gut
Reducing inflammation
Improving tolerance compared to live probiotics
Lower risk of gas, bloating and symptom flares
Because parabiotics do not replicate or ferment in the gut, they are often better tolerated, especially in the early stages of gut healing.
Probiotics, prebiotics or parabiotics: which is best?
There is no one-size-fits-all answer. Each plays a different role, and the right choice depends on the individual, their symptoms, and what is happening in their gut.
Probiotics can be helpful once the gut environment is ready to receive them and some gut healing has been completed.
Prebiotics are essential for long-term microbiome diversity but may need careful timing and dosing.
Parabiotics offer a gentler, more controlled way to support the gut and immune system, particularly in sensitive cases.
In my clinical work & inside my membership, the order, dose and combination matter just as much as the product itself.
Getting personalised gut support
If you experience bloating, pain, diarrhoea, constipation, food reactions or feel worse when taking probiotics or eating high-fibre foods, it’s a sign that there may be an underlying imbalance that needs addressing first.
Choosing the right probiotic, prebiotic or parabiotic — and knowing when to use each — requires an understanding of gut physiology, microbiome dynamics and individual tolerance.
If you would like personalised guidance, you can book a free 15-minute discovery call to discuss your symptoms and explore what approach may be most appropriate for your gut health journey.
Or jump on the waitlist for the Tummy Rescue Hub, to hear when doors open again:
More articles you might love:
Download my FREE E-book: 5 ways to reduce your bloating, pain & gas ☝️☝️☝️
The heartbeat
behind the work! 💚✨
🌿
I am Danielle Elliott a qualified Naturopath and the owner of Tummy Rescue.
I have been helping kids & adults improve their health for over 20 years, with the last 16 years concentrating on helping patients with any kind of gut disorder. I began focussing on everything gut related after my husband was diagnosed with Crohn’s Disease. And lucky I did……as my husband and both our kids have Coeliac Disease and my daughter has a dairy protein allergy.
So…. I am well and truly where I am meant to be!
I love being able to help people to soothe and calm their symptoms, investigate the causes and support and improve their gut function.
I also get to write educational pieces to train practitioners and am often interviewed for podcasts and summits, which is another really rewarding part of my work. I love educating people (this is something I do in every consult), because I do believe knowledge is power. It gives you the tools to make the changes you need to!
So, when you opt-in to my E-book, you are beginning on a journey of learning and discovery, of how you can reduce your symptoms of bloating, gas & pain and improve your gut health.
I would be honoured to help you along the way.
Danielle ✖️🧡✖️🧡